|
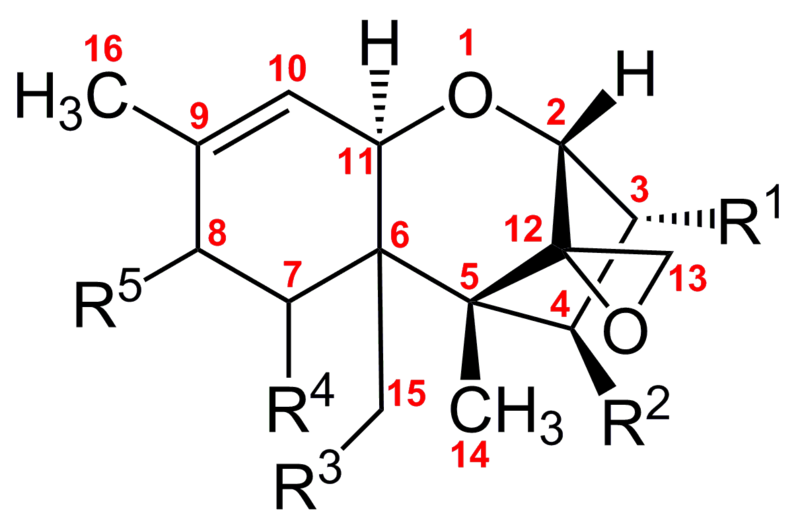
Mycotoxins are secondary metabolites produced by microfungi that are capable of causing disease and death in humans and other animals. Because of their pharmacological activity, some mycotoxins or mycotoxin derivatives have found use as antibiotics, growth promotants, and other kinds of drugs; still others have been implicated as chemical warfare agents. This review focuses on the most important ones associated with human and veterinary diseases, including aflatoxin, citrinin, ergot akaloids, fumonisins, ochratoxin A, patulin, trichothecenes, and zearalenone. Mycoses and Mycotoxicoses Fungi are major plant and insect pathogens, but they are not nearly as important as agents of disease in vertebrates, i.e., the number of medically important fungi is relatively low. Frank growth of fungi on animal hosts produces the diseases collectively called mycoses, while dietary, respiratory, dermal, and other exposures to toxic fungal metabolites produce the diseases collectively called mycotoxicoses. Mycoses range from merely annoying (e.g., athlete's foot) to life-threatening (e.g., invasive aspergillosis). The fungi that cause mycoses can be divided into two categories, primary pathogens (e.g., Coccidioides immitis and Histoplasma capsulatum) and opportunistic pathogens (e.g., Aspergillus fumigatus and Candida albicans). Primary pathogens affect otherwise healthy individuals with normal immune systems. Opportunistic pathogens produce illness by taking advantage of debilitated or immunocompromised hosts. The majority of human mycoses are caused by opportunistic fungi (149, 172, 245, 265). The mechanisms of pathogenesis of both primary and opportunistic fungi are complex, and medical mycologists have devoted considerable research energy trying to identify the factors that distinguish fungal pathogens from saprophytic and commensal species (31, 66). Some infections remain localized, while others progress to systemic infection. For many mycoses, the ordinary portal of entry is through the pulmonary tract, but direct inoculation through skin contact is not uncommon. In contrast to mycoses, mycotoxicoses are examples of “poisoning by natural means” and thus are analogous to the pathologies caused by exposure to pesticides or heavy metal residues. The symptoms of a mycotoxicosis depend on the type of mycotoxin; the amount and duration of the exposure; the age, health, and sex of the exposed individual; and many poorly understood synergistic effects involving genetics, dietary status, and interactions with other toxic insults. Thus, the severity of mycotoxin poisoning can be compounded by factors such as vitamin deficiency, caloric deprivation, alcohol abuse, and infectious disease status. In turn, mycotoxicoses can heighten vulnerability to microbial diseases, worsen the effects of malnutrition, and interact synergistically with other toxins. The number of people affected by mycoses and mycotoxicoses is unknown. Although the total number affected is believed to be smaller than the number afflicted with bacterial, protozoan, and viral infections, fungal diseases are nevertheless a serious international health problem. Mycoses caused by opportunistic pathogens are largely diseases of the developed world, usually occurring in patients whose immune systems have been compromised by advanced medical treatment. Mycotoxicoses, in contrast, are more common in underdeveloped nations. One of the characteristics shared by mycoses and mycotoxicoses is that neither category of illness is generally communicable from person to person. Mycoses are frequently acquired via inhalation of spores from an environmental reservoir or by unusual growth of a commensal species that is normally resident on human skin or the gastrointestinal tract. These commensal species become pathogenic in the presence of antibacterial, chemotherapeutic, or immunosuppressant drugs, human immunodeficiency virus infection, in-dwelling catheters, and other predisposing factors (31, 66). The majority of mycotoxicoses, on the other hand, result from eating contaminated foods. Skin contact with mold-infested substrates and inhalation of spore-borne toxins are also important sources of exposure. Except for supportive therapy (e.g., diet, hydration), there are almost no treatments for mycotoxin exposure, although Fink-Gremmels (80) described a few methods for veterinary management of mycotoxicoses, and there is some evidence that some strains of Lactobacillus effectively bind dietary mycotoxins (72, 73). Oltipraz, a drug originally used to treat schistosomiasis, has been tested in Chinese populations environmentally exposed to aflatoxin (111). In plant pathology, many secondary metabolites produced by bacteria and fungi are pathogenicity or virulence factors, i.e., they play a role in causing or exacerbating the plant disease. The phytotoxins made by fungal pathogens of Cochliobolus (Helminthosporium) and Alternaria, for example, have well-established roles in disease development (287), and several mycotoxins made by Fusarium species are important in plant pathogenesis (62). On the other hand, there is relatively little evidence that mycotoxins enhance the ability of fungi to grow in vertebrate hosts. Aspergillus fumigatus is case in point. It is the major species associated with aspergillosis and produces gliotoxins (inhibitors of T-cell activation and proliferation as well as macrophage phagocytosis). However, gliotoxin is not known to be produced in significant amounts by Aspergillus fumigatus during human disease (265). On the other hand, there are reports that gliotoxin has been associated with infections by Candida albicans (230, 231). The ability to grow at human body temperature (37°C) is clearly an important requirement for systemic mycotic infection, but the optimum temperature for the biosynthesis of most mycotoxins is within a more mesophilic range (20 to 30°C). For this and other reasons, the current view is that while some mycotoxins are known pathogenicity factors in plants, their significance in human mycoses is not yet clear.
Definitions, Etymology, and General Principles The term mycotoxin was coined in 1962 in the aftermath of an unusual veterinary crisis near London, England, during which approximately 100,000 turkey poults died (22, 82). When this mysterious turkey X disease was linked to a peanut (groundnut) meal contaminated with secondary metabolites from Aspergillus flavus (aflatoxins), it sensitized scientists to the possibility that other occult mold metabolites might be deadly. Soon, the mycotoxin rubric was extended to include a number of previously known fungal toxins (e.g., the ergot alkaloids), some compounds that had originally been isolated as antibiotics (e.g., patulin), and a number of new secondary metabolites revealed in screens targeted at mycotoxin discovery (e.g., ochratoxin A). The period between 1960 and 1975 has been termed the mycotoxin gold rush (157) because so many scientists joined the well-funded search for these toxigenic agents. Depending on the definition used, and recognizing that most fungal toxins occur in families of chemically related metabolites,. some 300 to 400 compounds are now recognized as mycotoxins, of which approximately a dozen groups regularly receive attention as threats to human and animal health (49). Mycotoxicoses are the animal diseases caused by mycotoxins; mycotoxicology is the study of mycotoxins (84). While all mycotoxins are of fungal origin, not all toxic compounds produced by fungi are called mycotoxins. The target and the concentration of the metabolite are both important. Fungal products that are mainly toxic to bacteria (such as penicillin) are usually called antibiotics. Fungal products that are toxic to plants are called phytotoxins by plant pathologists (confusingly, the term phytotoxin can also refer to toxins made by plants; see Graniti [93] for a cogent discussion of the etymology of phytotoxin and its use in plant pathology). Mycotoxins are made by fungi and are toxic to vertebrates and other animal groups in low concentrations. Other low-molecular-weight fungal metabolites such as ethanol that are toxic only in high concentrations are not considered mycotoxins (10). Finally, although mushroom poisons are definitely fungal metabolites that can cause disease and death in humans and other animals, they are rather arbitrarily excluded from discussions of mycotoxicology. Molds (i.e., microfungi) make mycotoxins; mushrooms and other macroscopic fungi make mushroom poisons. The distinction between a mycotoxin and a mushroom poison is based not only on the size of the producing fungus, but also on human intention. Mycotoxin exposure is almost always accidental. In contrast, with the exception of the victims of a few mycologically accomplished murderers, mushroom poisons are usually ingested by amateur mushroom hunters who have collected, cooked, and eaten what was misidentified as a delectable species (184). Mycotoxins are not only hard to define, they are also challenging to classify. Due to their diverse chemical structures and biosynthetic origins, their myriad biological effects, and their production by a wide number of different fungal species, classification schemes tend to reflect the training of the person doing the categorizing. Clinicians often arrange them by the organ they affect. Thus, mycotoxins can be classified as hepatotoxins, nephrotoxins, neurotoxins, immunotoxins, and so forth. Cell biologists put them into generic groups such as teratogens, mutagens, carcinogens, and allergens. Organic chemists have attempted to classify them by their chemical structures (e.g., lactones, coumarins); biochemists according to their biosynthetic origins (polyketides, amino acid-derived, etc.); physicians by the illnesses they cause (e.g., St. Anthony's fire, stachybotryotoxicosis), and mycologists by the fungi that produce them (e.g., Aspergillus toxins, Penicillium toxins). None of these classifications is entirely satisfactory. Moreover, as our anthropomorphic focus shifts attention, the same compound may get placed in different cognitive cubbyholes. Aflatoxin, for example, is a hepatotoxic, mutagenic, carcinogenic, difuran-containing, polyketide-derived Aspergillus toxin. Zearalenone is a Fusarium metabolite with potent estrogenic activity; hence, in addition to being called (probably erroneously) a mycotoxin, it also has been labeled a phytoestrogen, a mycoestrogen, and a growth promotant. For this article, we will eschew classification and simply list the major mycotoxins in alphabetical order by name.
For example, mycotoxicoses, like all toxicological syndromes, can be categorized as acute or chronic. Acute toxicity generally has a rapid onset and an obvious toxic response, while chronic toxicity is characterized by low-dose exposure over a long time period, resulting in cancers and other generally irreversible effects (128). Accepting that it is often difficult to distinguish between acute and chronic effects, many papers on mycotoxicoses blur this basic dichotomy entirely, and it is not always easy to interpret the published data on purported health effects. Almost certainly, the main human and veterinary health burden of mycotoxin exposure is related to chronic exposure (e.g., cancer induction, kidney toxicity, immune suppression). However, the best-known mycotoxin episodes are manifestations of acute effects (e.g., turkey X syndrome, human ergotism, stachybotryotoxicosis). In order to demonstrate that a disease is a mycotoxicosis, it is necessary to show a dose-response relationship between the mycotoxin and the disease. For human populations, this correlation requires epidemiological studies. Supportive evidence is provided when the characteristic symptoms of a suspected human mycotoxicosis are evoked reproducibly in animal models by exposure to the mycotoxin in question (121). Human exposure to mycotoxins is further determined by environmental or biological monitoring. In environmental monitoring, mycotoxins are measured in food, air, or other samples; in biological monitoring, the presence of residues, adducts, and metabolites is assayed directly in tissues, fluids, and excreta (121). In general, mycotoxin exposure is more likely to occur in parts of the world where poor methods of food handling and storage are common, where malnutrition is a problem, and where few regulations exist to protect exposed populations. However, even in developed countries, specific subgroups may be vulnerable to mycotoxin exposure. In the United States, for example, Hispanic populations consume more corn products than the rest of the population, and inner city populations are more likely to live in buildings that harbor high levels of molds (5). Methods for controlling mycotoxins are largely preventive. They include good agricultural practice and sufficient drying of crops after harvest (153). There is considerable on-going research on methods to prevent preharvest contamination of crops. These approaches include developing host resistance through plant breeding and through enhancement of antifungal genes by genetic engineering, use of biocontrol agents, and targeting regulatory genes in mycotoxin development (26). As of now, none of these methods has solved the problem. Because mycotoxins are “natural” contaminants of foods, their formation is often unavoidable. Many efforts to address the mycotoxin problem simply involve the diversion of mycotoxin-contaminated commodities from the food supply through government screening and regulation programs. There is a vast literature on mycotoxins, and numerous monographs have been published (15, 16, 19, 47, 49, 64, 133, 136, 150, 162, 177, 211, 216, 235, 237, 246, 259, 283, 285, 286). In addition, there are hundreds of review articles and thousands and thousands of papers in the primary literature. Unfortunately, too many publications about mycotoxins consist largely of mind-numbing accumulations of assorted facts: lists of clinical manifestations in different animal species (both exposure tests in laboratories and veterinary diagnoses of mycotoxicoses in agricultural settings), compendia of different toxins found in different foodstuffs, comparisons of assay protocols, tables of international regulations governing mycotoxin levels, and so forth. There is also a significant literature addressing fundamental studies describing organic syntheses, elucidation of biosynthetic pathways, cloning of mycotoxin pathway genes, and other less applied aspects of mycotoxin research. The scientific quality of the mycotoxin literature is extremely variable. There is a disconcertingly high level of inaccuracy in a few reports, with some authors culling their information from earlier reviews of questionable merit and thereby perpetuating factual errors and discredited hypotheses. Where possible, we will attempt to point out such misinformation. We will focus on those mycotoxins that are known or suspected to cause human disease; on metabolites that are produced by molds that are associated with human food or habitation; and on other topics related directly to human health. Previous reviews on mycotoxins and human health include those by the Council for Agricultural Science and Technology (53), Robens and Richard (215), Beardall and Miller (7), Kuiper-Goodman (145), Fink-Gremmels (80), Peraica et al. (195), Hussein and Brasel (126), and Etzel (76). Because the field of mycotoxin research is so large and so fragmented, and because the criteria for establishing human mycotoxicoses are so elusive, the goal of this article is to give a simple introduction to clinical microbiologists. We will briefly describe what is known about the chemical structure and biosynthesis of the mycotoxin, list the producing fungal species, and give the clinical manifestations and toxicological profiles of the associated mycotoxicoses. In each case, we will refer the reader to selected pertinent papers from the primary literature as well as to other, more comprehensive reviews. SOURCE: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC164220/
Are mycotoxins considered VOC's? Mycotoxins and human disease: a largely ignored global health issue https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2802673/
How fungi defend themselves against microbial competitors and animal predators https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6126850/
Additional study, research and documentation on Mycotoxins
Things that fight or inhibit growth of deadly mycotoxins
|
|
Do you think you might have mold in your home, place of business or school? Are you or someone you love suffering from an unknown illness that doctors can't diagnose? Is mold making you sick? Go to our Step by Step and start Surviving Toxic Mold. |